Are we guilty of single factor thinking? Part one
We are often guilty of single factor thinking with regards to the body. X causes Y and therefore Z is the answer. We can blame an over-pronating foot or a glute that does not fire. We may look to a scan and accuse a bulging disc or a rip or tear in a rotator cuff. We may assess someone’s biomechanics and proclaim them as the source of their problems. It could be the timing of the activation of a fancy little muscle of your core. Hang on, wait a moment it could be your pesky fascia. It could even be the fancy bit of blancmange in your head that people are blaming more and more these days. My current favourite is muscles that facilitate and inhibit each other!
This happens all the time in the world of therapy and corrective exercise. We can get very attached to these apparent causes so much so that they are frequently a go to for whatever problem has reared its ugly head. Single factor thinking is often seen in a specific therapy or method also where only the teachings and skills learned from a particular guru or XXX (insert method here) are considered.
If we are honest we all have some cognitive biases we are each fighting against that are dictated by our educational influences and work experiences. After all you have dedicated time and often money into your current line of thinking. But we have to ask ourselves is it enough? And are we willing to adapt outside of our comfort zone and biases.
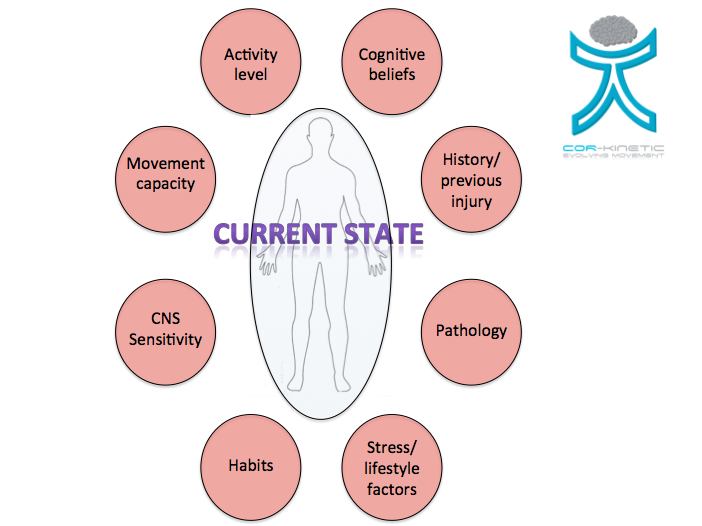
The point of this blog is that it is not always that simple and we have to entertain the idea that there maybe multiple influences acting in varying degrees on the current state of the individual rather than just a single factor. These contributors can be across the physical and cognitive realms and could explain why pain can come and go or improve or worsen seemingly inexplicably. It may explain why people gain and lose weight even though they seem to be maintaining the same level of exercise and intake of food.
If there are contributing factors that we have not thought of as contributing factors and that cease to be so this may impact positively on the overall pain experience. If we are only thinking of the physical or mechanical aspects that might cause pain then this may not factor in our thought process. Equally if we are more based in the cognitive or neurological side we may think more about the processing or psychological side of pain than things like current activity levels as an example.
In the diagram above are some of the factors that could impact on the current state of the individual.
It might be a bit like watching one of these air disaster programs. There always seems to be multiple factors that contribute to the disaster. Maybe the weather was bad and compounded by the fact the deicing system was down, this might be coupled with missing an air traffic control instruction or an instrument that was faulty. The variables are endless but all are taken into consideration because of the realization that multiple factors could possibly be at play.
Tom Goom of www.running-physio.com posted a cartoon on twitter @tomgoom a little while ago that kind of summed this up and provided a genesis for this blog. The neurocentric model can suffer from single factor thinking as much as a pathology-biomechanical model. For a subject as complex as pain you have to be pretty well rounded to consider all the possible contributing factors.

You have probably had that short leg all your life that is apparently causing your back pain but the pain in your back comes and goes? Your ‘’biomechanics’ may have been bad forever and do we regularly see feet that have recently become spontaneously flat?
Now even though we do not see these things associated consistently with pain in the literature, even if they were for arguments sake causing a problem then the question is why now? Why now when they have been knocking around for all these years? Why can the problems be so inconsistent if the apparent cause is structurally consistent?
People with pain in just one Achilles tendon can have structural changes in both Achilles tendons that maybe associated with pain and may never develop pain in the asymptomatic tendon. *Click Here*
We see a high prevalence of asymptomatic rotator cuff tears. So we have to ask the question why do the cuff tears that hurt, hurt? It can’t just be the physical damage that is seen on the imaging. *Click Here*
The gap between tissue damage and the level of pain experienced is becoming wider and wider the more we research. As we embrace the role of the central nervous system we also have to consider all the factors that may influence the CNS. This paper from Littlewood et al *Click Here* does a good job in discussing other factors with regards to the rotator cuff.
The issue here is that in a unclear world we cannot always expect a clear cut answer or cause to be easily and consistently available. Instead a multifactorial model maybe necessary when considering an individuals current state.
In This first blog we will look at two of the most important.
- Stress
- Activity level
Stress
On an anecdotal level many of us have experienced increased pain in times of stress. That neck or back ache that rears its head in times of emotional or work related stress. You may have also seen it with your patients or clients.
This could be a direct stress response due to an injury that may have arose from a sense of disability the injury has caused us. We also have physiological stressors from our increasingly manic lives that may maintain a pain state.
Decreasing catastrophizing over either an acute or chronic injury through an increase in education about both normal and maladaptive pain responses may decrease stress. Education about how to manage external stressors such as job, lifestyle or emotional related factors can also be successful in decreasing stress.
Whether you are a physio, trainer or yoga instructor, stress can impact on what you are trying to achieve with your patient or client.
On its own stress may not be enough to cause pain but might be a contributing factor in the complex pain puzzle where we see a relationship between injury, pain and stress.
The disruption of homeostasis on both a physical tissue and a neural level in a pain state leads to responses to restore stability or homeostasis. Melzack in his “Pain and the Neuromatrix in the Brain” paper *Click Here* discusses the link between pain and stress in detail. One output of the neuromatrix is stress regulation programs that involve cortisol and noradrenalin levels in response to external stressors, either psychological or physiological, that input into the neuromatrix. The increased output of cortisol is proposed by Melzack to have a cumulative destructive effect on muscle, bone and neural tissue.
These stress factors in chronic pain are starting to be explored. This paper *Click Here* found increased level of stress hormone cortisol in chronic back pain patients. The authors suggesting that a sustained endocrine stress response may contribute to persistent pain states.
The adaptation to stressors that involves the neural and neuroendocrine involved in the restoration of homeostasis is called allostasis and describes our internal variability to achieve homeostasis. Long-term stress responses are more common in today’s environment than the episodic short-term fight or flight survival responses that may have been involved in more primal situations. Sapolsky discusses this in detail in his book “Why Zebras don’t get ulcers” and the increased risk of disease and disability.
The long-term biological consequence of these types of chronic stressors to the body is called the allostatic load. Although we are adaptable and variable it is hard to maintain an overload of this nature indefinitely without some form of problem developing.
Borsook et al in this paper *Click Here* discuss the maladaptive stress response or the allostatic load with regard to migraines. Specific stressors linked to migraines include psychological/emotional and physiological factors such as work, anxiety and noise and light.
Conditions that lead to allostatic load are:
- Repeated frequency of stress responses to multiple novel stressors
- Failure to habituate to repeated stressors of the same kind
- Dysregulation of Normal Adaptive Responses
Coupled with other factors contributing to the current state of the individual the activities of the stress systems will contribute to the CNS processing of pain (Butler – Sensitive nervous system)
Physical activity itself is a stressor that has physiological effects coupled with psychological stress would increase the overall stress response. Here we see both as possible contributors to the current state.
Adrenaline another regulatory hormone of the endocrine system is released with mental stress (Lundberg *Click Here*) Adrenaline can act as a central excitatory neurotransmitter that may amplify afferent information (Butler). We see increased adrenaline secretion during exercise.
Activity level
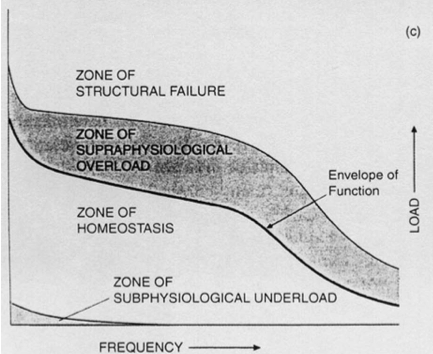
Homeostasis is as important for our physical tissues as it is for stress systems. Our activity levels must keep within the loading ability of the tissue for the body to be able to deal successfully with the load. This has been labeled the zone of homeostasis by Dyer in this paper *Click Here* on the pathophysiology of patella femoral pain. The outer limit being defined as the envelope of function.
He describes this as “the force (torque) that can be safely withstood and transmitted by that system without damage”
Prolonged exposure to the zone of supraphysological overload (diagram above) loading may create nociceptive (noxious stimulus – Chemical or mechanical) output from the structures of the knee unable to accept the level of loading. This could be caused by excessive long distance running for example. With a runner this would be a major component to any reasoning process behind a cause of pain. I think this is what Tom Goom was kind of getting at with his cartoon. The nociception generated by tissue overload would certainly be a major contributor the current pain state. A way of reducing the current pain state may simply be to bring the level of load back within the zone of homeostasis.
Many running injuries are seen to be the result of too much to soon in many cases and weighting of any reasoning would have to appreciate this. In some situations however this may not be the case with symptoms continuing even after a long durations of rest or proving to be unpredictable.
Some days the pain can feel better and other days worse and this maybe with exactly the same loading. Suddenly the pain seems almost to be gone to then spring back with vengeance. Imagine if the problem has been going on for quite a while and you felt like you may never run again. Any twinge in that knee might spell catastrophe. Suddenly we become hyper vigilant with every step amplifying the sensation. When we have a prolonged collective firing of neurons involved with a movement, a pain and emotion we can start to form negative neural patterns that are reinforced and become hard to break.
Nociception or noxious stimulus is one input from the body into the neuromatrix. The brain then assesses the level of danger and outputs a response such as the sensation of pain or a decrease in movement. Nociception neither being necessary nor sufficient for pain.
Therefore other factors acting on the system such as stress levels, attitudes and beliefs about pain or previous pain experiences may amplify or attenuate the actual painful experience rather than a simple relaying of the state of the tissue. The homeostasis of the tissue and the processor of the input from the tissue the brain are intimately intertwined. Nervous system issues such as peripheral or central sensitization may change the message the brain receives, as could an increase or decrease in descending inhibition alter the resultant pain output.
The load to the tissue will be of upmost importance especially with an athletic population but it does not mean that it is the only factor affecting the current state. With a runner both knees will be under similar physical loading but often only one will hurt.
This could be to do with motor control or biomechanical issues but not always. These would be contributing factors to consider but with the best mechanics in the world you may still be running to much or have a jumpy nervous system from a previous pain experience or a belief from a previous injury and some information acquired. Equally pain is not just “in the brain” which implies no relationship with the tissue.
This may lead the single factor thinker to scratch their head or blame the outlier, the patient or client, to their thought process. This should drive the inward reflection of our skill set although this may not always happen.
The point of the blog is to consider and educate ourselves even on a superficial level into the many things that could impact on the current state of who we are dealing with in.
In the next part we will look at the other factors that can affect the current state of the individual.