Do you need your joints to be 'centered'? – Does it really matter?
One of the subjects that has cropped up recently a few times in our courses and also in some of the articles I have read is the theory of ‘joint centration’ or a 'neutral' joint positioning.
The theory is that it is advantageous to have a neutral joint 'position' or axis of rotation to work from to allow us maximal capacity to rotate around the joint. With a joint 'centered' we will be able to move equally in all directions rather than having reduced movement capacity from being positioned towards one end of the joints range. It is proposed to reduce the mechanical stress to the joints and tissues and also allow optimal load transference. This idea is a crucial component to many schools of thought.
Now I really like the idea and it makes a lot of sense from a mechanical perspective. However one of the biggest lessons I have learned over the last few years is that not everything that makes sense turns out to be true or makes that much sense when we see the body as less mechanical, unpredictable and highly individual.
Joint centration is proposed to happen via a precise and coordinated sequence and timing of muscular activation that has been defined in theoretical models. Through this process we can achieve ‘optimal’ or ‘ideal’ movement.
As I suggested before this sounds great but:
- Does it matter if your joint aren’t centrated?
- Can we link this lack of centration to pain and injury?
- Is the theory supported by the research?
- Can we find a consistent activation patterns that are either positive or negatively correlated?
- Do we know what optimal/ideal movement really is?
To explore these questions we will have to look at two key issues in this blog:
- Static and dynamic postures
- Sequence and timing of muscle activation
If these factors, that would affect the joints neutral position and therefore mechanical advantage and proposed excess tissue stress, have a bearing on pain or injury then we would see a correlation between the two factors.
First off lets look at a correlation between people in pain and their posture.
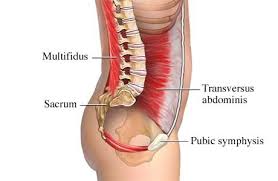
Your static posture would have an effect on the starting position of your joints as we see in the diagram above and has been proposed to create stress to the tissue and even stress to the central nervous system (although I could find no evidence to support this).
Equally though we must be mindful that the end position is also important. This will give us an idea of how much movement is available. We could have a perfectly aligned posture but is this pointless without the ability to move? Equally stability is unimportant without mobility, neither maybe more important than the other but instead have a symbiotic relationship.
If joint alignment were important surely this would be well supported in the literature?
I see this subject a little like overpronation. Lots of people have feet that overpronate but they still get no pain, run marathons and are involved in high-level sport.
How many people have what may be regarded as ‘bad’ postures and possibly accompanied by a lack of joint centration, both statically and dynamically, but get no pain?
We will often herald peoples amazing compensatory abilities for various postural and structural ‘anomalies’ through their tissue tolerance, reflexes and strength for example but surely everybody who does not get pain or injury from poor joint alignment does not fall into the extra ordinary category?
Posture
Enough of my opinion though! Lets look at what we have available in the research. There is far more available with regards to static posture so we will start there.
This study looked at the correlation between cervical spine posture and neck pain. *Click Here*
The researchers took two groups, one with neck pain and one without. They measured both the global angles and segmental angles of the cervical spine and then measured them against neck pain suffered.
There were no significant differences between the postures of the group with neck pain vs the group without. The average segmental angle at the kyphotic level was 6.5° in the pain group and 6.3° in the group without pain
One of the problems here is that they had no standard values for normal and therefore if deviation from normal posture was a factor in neck pain. This is a consistent problem when looking posture and movement is trying to define what is normal in the first place. If we have no normal then what is ‘bad’ and what is ‘good’?
Another study looked at the changing posture of children between 5 & 6 and 15 & 16 *Click Here*
During the 10-year period of this longitudinal study we see a significant change in the posture and mobility of the subjects spines. With this change in posture we should see a change in pain levels if the two correlate and 38% of the 15-16 year olds complained of lower back pain on occasion. However the researcher’s reported no correlation between posture, spinal mobility or physical activity and the pain.
This study *Click Here* looked at back pain amongst former and current elite gymnasts. Both reported back pain. 27% of the former and 38% of the current gymnasts but the researchers found no correlation between posture, range of motion and reported back pain.
Here *Click Here* the spinal postures of acute, chronic and healthy groups were studied. We certainly see postural changes with age and increased body mass but no significant differences in posture of any of the three groups with regards to pain.
Leg length discrepancies (LLD) have long been hypothesized to throw out our posture all the way up the kinetic chain and therefore the position and amount of available joint motion we would have. In fact Google images is simply awash with pictures *Click Here* showing us the consequences on our posture.
This study *Click Here* found no link between unequal leg length and back pain and this study *Click Here* found minimal effect on pelvis and spine kinematics from a LLD.
Are your postural and joint positions simply related to the activation of muscles around a joint anyway? It would seem from a great deal of literature that our postural positions are governed by a complex interplay between our visual, vestibular and sensory motor systems. Retraining the activation or sequence of activation of the muscles around a joint may have no effect if our posture is being influenced by other factors.
So our static posture certainly will influence the fixed axis of rotation around a joint. The point here is does our posture have an effect on our pain and based on the available evidence I could not conclude that it does.
Dynamic posture is a far more complicated subject. Our dynamic posture would surely be determined by the task we are performing often with a large amount of variation during execution.
Here we need to start to look at the instantaneous axis’s of rotation instead of a simpler fixed axis that we would see with a static posture to maintain an ‘optimal’ mechanical advantage at the joint. Now this concept certainly challenges my grey matter as it is pretty complicated mechanical stuff! There is also far less research that we can look at with regard to dynamic posture.
An instantaneous axis occurs when we have a moving body that is translating and rotating, so during actual dynamic movement rather than more clinical situations.
When we have an instantaneous axis we can assume that the motion around the joint is pure rotation. To achieve this the translation element of the bones would need to be concurrent to keep the close association. The problem is that we know the body’s movement is sequential and to achieve any kind of range of movement would have to be accumulative. Large ranges of movement of the body being the accumulation of range from multiple joints. Spinal motion is a good example; each segment has a small amount of range that adds up to a larger range of movement across the entire structure.
A function related example would be reaching for a tennis shot or lunging for a tackle in football. Your joints would need to be out of centration often to achieve the range the task requires repetitively throughout a match and a career. You may not get injured keeping them centrated but you may also find it hard to play the game and I am yet to see proof of lack of centration being a cause of injury in professional sport. I see this as a classic example of a clinical idea of movement in a functional world. It may help to teach the central nervous system to move multiple segments in a coordinated fashion in functional contexts and specific movements to keep close association of the segments.
The issue here is that each movement would need to be individually trained to create the specific motor coordination between segments that is required as the synergistic relationship would be constantly altering according to movement, joint angle, speed and the position of the other associated body segments. There maybe no ‘correct’ or ‘ideal’ muscular synergistic pattern as we will discuss shortly.
We also have to realize that these motions at a joint are very small and I suspect people have restricted range in many joints that cause no pain at all.Natural anatomical variation may also restrict the ability for a joint to be centrated. If you are structurally unable to achieve ‘neutral’ does this become an individual ‘neutral’? If not then we would all be in trouble with the huge amount of anatomical variation between humans.
So it is certainly clear that our dynamic or static postures would exert a large influence on the position of a joint and the ability to start from, maintain and return to a centralized or neutral position. Can it simply be related to pain or injury? This maybe less clear.
This all does not mean that in many sports that require very technical movements such as weightlifting or golf that body alignment is unimportant, far from it. We still see wonderful movers such as Roger Federer who suffered from back pain or Bubba Watson with what could be described as a less than ideal swing still winning Majors and keeping relatively injury free. This is also mirrored outside of the sporting world.
“Correct” muscle activation
Another part of the theory behind good joint positioning is the precise and coordinated activation of muscles in a specific sequence.
I attempted to find specific muscular activation patterns that consistently correlated with either painful or healthy subjects to find out if muscle activation patterns did happen in a uniform way that had positive or negative outcomes.
There is a whole bunch of theory available to read here and so a great place to look to is the research for a more objective view of whether we see precise patterns emerge and if they correlate with pain.
Lets look first at the prone leg extension test to evaluate muscle firing of the lumbopelvic region. This test is performed the world over by therapists and trainers trying to find out if your ‘glutes’ are firing by someone lying down on their front and the therapist/trainer sticking their fingers into various parts of the anatomy.
Firstly remember please that our fingers are not expensive EMG electrodes sensitive enough to pick up and quantify the millisecond changes in muscular onset, especially through the layers of subcutaneous fat that may be a little thicker in some. It is very difficult to know what is happening internally in the human body outside of a lab. This is true for biomechanics as well as muscle function.
Secondly do we actually know what the correct firing pattern is? The theory is that your glutes should fire before your hamstrings that fire before your lower back. This prone test is meant to recreate what happens during your hip extension during gait and hopefully reduces the amount of extension created from the lumbar spine.
A consideration is does a test lying prone give us a good idea of your muscular activation performance in another context such as walking or running when are upright and have multiple body segments interacting with gravity and ground reaction forces?
Interestingly for such a well known theory there is not a whole bunch of research into this. Lieberman et al *Click Here* looked at the glutes role in running and walking. We see significant differences between the two in both activation levels and timings of activation. Which are we testing for in the prone hip extension test? This also shows that muscle function can be variable in different tasks. In fact there was no obvious peak to the EMG signal during walking gait as we may expect with the glutes ‘firing’ as the hip extends.
Lehman et al tested the theory of correct activation in the muscular sequence as discussed above *Click Here* They found in asymptomatic people there were no consistent recruitment patterns and variability was seen across the subjects. There was a large range between the onset times of muscles. Previous studies also did not correlate with the theorized ‘correct’ order of muscle activation.
Core stability was also hypothesized to be about the correct order and timing of muscle activation, You can read my review of the efficacy of a core stability approach to back pain *Click Here*
Vasseljen et al *Click Here* found that firstly there was a large variation in abdominal muscle activation and secondly it was unaffected by 8 weeks of abdominal training.
Mannion et al *Click Here* found that baseline measures of neither abdominal function nor improvements had any affect on a good clinical outcome.
So can we change timing? Do we know what the ‘correct’ timing is? Does it have any affect on pain?
Certainly this would not give us an unequivocal answer. The age-old argument to the contradictory or unclear evidence is often:
- They did not perform the study correctly for XXX reason.
- Our theory is different.
- In our clinical experience we see XXX.
The onus here then would be to provide the evidence to back up the theory or specific method to prove beyond doubt the efficacy of the approach.
We have given muscles specific roles such as stabilizers and prime movers that play an important role in the ‘joint centration’ theory. We can certainly hypothesis what a muscle is supposed to be doing and when it should be doing it. It is a little harder to know for sure though really what is happening internally and if a single muscle not doing its theorized ‘job’ is it as catastrophic as some make out?
One of the ways we have tried to define a muscles role is through its fibre type distribution. If it has more slow twitch fibres we may classify it as a postural or stabilizing muscle and more fast twitch then it is more of a moving muscle. In reality all muscles maybe more synergists if we look at different theories. We will get to that in the next section.
T. Haggmark et al *Click Here* found that the predominant fibre types of the core muscles, (rectus abdominis, RA, obliquus externus, OE, obliquus internus, OI, and transversus abdominis, Tr), varied very little between the different muscles of the individual leading them to conclude that they have a very similar functional capacity. There were large inter individual variations however. This study here *Click Here* although a little confusing in places found “no preponderance of either fibre type” in most of the 36 muscles studied.
Thus muscle fibre type distribution appears, like most things, to be hugely variable to the individual. Genetics, gender and activity type and levels seem to play a role in individual distribution. Many muscles seem to a have a roughly equal split of fibre types. Does this make it harder to then label them with specific roles?
Other theories
Another theoretical, and possibly oppositional, idea would be that of dynamic systems theory. Here we see the idea that variability in muscle activation is perfectly normal and healthy.
Davids et al *Click Here* see trial to trial movement variations as healthy, omnipresent and unavoidable. This variation has been supported by the studies in this blog and may not be consistently relevant in the pain experience. This study highlight that skilled movers have more variability while less skilled rigidly fix their movement strategy *Click Here*
Falla et al *Click Here* found that during a lifting task healthy individuals actually displayed more variation in intra muscular activity vs. back pain subjects who exhibited a consistent strategy of muscular activation. In this case intra muscular activation variability during a repetitive task maybe healthy rather than a specific activation pattern.
In the healthy participants section of the graphic on top we see a shift in the activation of the lumbar erector spinae from the cranial towards the caudal section of the muscle. The pain group below only activates a similar region of the muscle. This may highlight both reduced motor variation and increased physiological stress.
We also have the problem of muscular redundancy. We have a large variation of musculoskeletal elements that the central nervous system can use to perform the same physical action. Any number of combinations of core muscle activation patterns or synergies could actually achieve the same task of spinal stability for example if required.
We activate muscles in synergies or groups to achieve tasks. The idea in therapy and fitness worlds of a single muscle achieving a task has never made sense to me given the muscular resource available. The individual timing and sequence of these synergies from EMG studies appears to be variable to the individual rather than clear patterns in health and unhealthy subjects emerging in the areas discussed so far in this piece.
So which activation pattern in a muscular synergy out of the many should we use? Which are redundant? Well modern motor theory such as “Uncontrolled Manifold Hypothesis” or an easier UMH approach looks at making use of the available redundant elements rather than seeking to restrict them. To read more *Click Here*
Specific patterns and timing of muscular activation again do not appear to be clear and in the case of lower back pain and core stability even relevant or changeable. Even a simple concept such as the agonist and antagonist to balance force to centrate a joint becomes even more complicated when we look at complex function related biomechanics. As a joint moves through three dimensions we would have to see a agonist and antagonist in each plane rather than the simplistic two dimensional model we currently work off.
Although it makes sense on a mechanical level to have joint centration, and therefore increased capacity, we may find it difficult to ‘correct’ muscular recruitment patterns if we have no real way of knowing what to correct them too. It also seems hard to blame the wrong muscular activation or postures for pain or injury if we see no definitive correlating patterns.
It is a clear help when we can have some objective data to work with when discussing the internal workings of the body. It becomes infinitely more difficult when we do not. We have to ask our selves what do we really know?